 |
| Tom Koch |
Executive Director, Euthanasia Prevention Coalition
An excellent research article was written by Tom Koch and published on February 12, 2022 titled: A Sceptics Report: Canada’s Five Years Experience with Medical Termination (MAiD).
Koch, who is an ethicist and long-time researcher on issues related to end of life care, examines Canada's experience with euthanasia in comparison to other jurisdictions that have legalized euthanasia and assisted suicide.
Koch thoroughly examines the history that led to the legalization of euthanasia (MAiD) in Canada and compares Canada to other jurisdictions, such as the Netherlands.
With reference to Canada Koch writes:
The Canadian experience since 2016 has evidenced a similar pattern of expansion. The annual number of cases increased annually as the class of potential recipients expanded. The Second Annual Report on Medical Assistance in Dying in Canada, 2020 reported that between 2016 and 2020 the number of reported cases of medical termination increased from 1018 to 7589. ... The result provincially and nationally has been the very definition of a slippery slope with an increasing number of cases whose individuals had a progressively broader set of medical conditions.To illustrate his point Koch writes:
In 2018, Canadian newspapers reported favourably on the medically induced deaths of George and Shirley Brickendens. In their 90’s, both were in reasonably good health, pain-free, and comfortably situated in a retirement home. Their existing chronic conditions were well managed medically and posed no immediate threat of serious decline. They sought and received MAiD not because they were in pain or particular distress but because they feared a future disabling illness. In the medical assessment required by law one doctor wrote that Mr. Brickendens, “has a serious and incurable illness, which is age-related frailty. It is end stage”. This ageist diagnosis was the physician’s way of fitting a stable, reasonably healthy patient with some chronic conditions into the broad, legal standard of candidacy.Koch then comments on circumstances where euthanasia might be considered for people who only fear future suffering. He continues by writing on an experience he had with a treatable patient who had requested euthanasia. Koch writes:
A similar fear was that MAiD would become a default clinical response in cases where treatment would otherwise be recommended. In 2020, for example, I was asked to consult for a 93-year-old woman in Toronto living independently with some home assistance whose bursitis prevented her from dressing and washing herself. She told an attending physician if she could not do those things she did not wish to live. She was then referred for assessment as a candidate for MAiD. Upon examination with a palliative care physician, however, we determined her bursitis could be easily treated thus permitting her to regain shoulder-arm function. With treatment her request was withdrawn and she died naturally several years later.Koch examines euthanasia of people with a wrong diagnosis. He first comments on the fact that of 133 people who Jack Kevorkian helped to kill, there were 88 autopsies and 3 of those autopsies indicated that there was "no evidence of any chronic, progressive disease." Koch then refers to an Australian study which found that 10% of people who ask for MAiD will have a misdiagnosis.
Koch continues by referring to a Canadian study on lung cancer patients that found that people diagnosed with lung cancer will often forgo effective life-saving treatment and immediately seek euthanasia. Koch writes:
In a recent report at the World Conference on Lung Cancer, Canadian researchers reported that with the increased accessibility of MAID, “Patients are seeking this option despite the availability of more effective and more tolerable treatment options. … While biomarker-driven, targeted therapies and other immunotherapies can be effective, many patients undergo medial termination without “accessing—or, in some cases, without being assessed for—these treatment options"Koch then examines the reason why Canadians are asking for euthanasia. Koch states:
The Health Canada report emphasizes the degree to which those seeking MAiD were concerned with the limiting effects of their conditions (84.9%) and a resulting loss of ability to perform daily activities (81.7%). That is, some say, while life might be lived it would not a life they wish to pursue. The suggestion that this is simply a logical and rational choice assumes that those limits are necessarily unmanageable.
Koch then states that some people are seeking euthanasia (MAiD) due to a lack of medical or community supports. He refers to a study by Gallagher et al. that argued, that a “hastened death” chosen because of disease burden and resulting distress is a medical error in the absence of “timely, quality palliative care.”
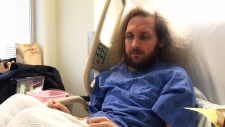 |
| Roger Foley |
In the most recent case to gain notoriety, 42-year old Roger Foley’s battle with the Health Science Centre’s Victoria Hospital in London, Ontario, is instructive. Foley has a degenerative neurological condition requiring skilled home support. Health authorities contracted with a private, for-profit company to provide his at-home care. The result of untrained, unsupervised personnel was, Foley charged, repeated hospitalizations. “I have been given the wrong medications, I have been provided food where I got food poisoning, I’ve had workers fall asleep in my living room, burners and appliances constantly left on, a fire, and I have been injured during exercises and transfers,” Foley claimed. “When I report these things to the agency, I would not get a response” (CTV 2018). The case became a cause celebre among disability rights advocates when Foley refused to leave the relative safety of his hospital bed and sued for the right to chose his own home care providers (Foley and Victoria Hospital et al. 2018). He became a national figure after tape recording a hospital ethicist suggesting he might consider medical termination instead of seeking better home care.Koch then seeks to open a wider discusion. He states:
Clearly, on the evidence, skeptics expectation of a slippery slope along with an increasing number of persons in an expanding class of eligible persons would seek and receive early medical termination was justified. The number of persons accessing medical aid in dying has expanded to include those who are simply afraid of future illnesses as well as those whose condition seems to them untenable in the absence of necessary services. And, too, there are those who might live with appropriate care and cognitive, physical, or sensory limits who simply refuse to accommodate the changes that would require. The critical concern of early skeptics that medical termination would become a substitute for the kind of palliative and other services the Senate Committee called for in 1995 has been fulfilled. MAiD is increasingly a default choice offered, and in some cases promoted, in areas where expert care and support are unavailable and sometimes even where they are available.Koch then discusses conscience rights and the pressure within the health care system to provide euthanasia. He writes:
Undiscussed here but not unimportant has been the manner in which practitioners and institutions have been pressured to provide MAiD assessments and service. Much of the evidence is anecdotal... But the defunding of a Delta, British Columbia, hospice that refused to provide MAiD, available at a hospital literaly next door, is one indicator of the pressures brought on those concerned that medical termination may be inappropriate.Koch argues that the lack of proper end-of-life care has made MAiD a choice for many people. He states that some people will suggest that what is done is done, but Koch argues the point. He states:
First, by introducing MAiD without attention to the necessities of care for those with chronically limiting, often painful progressive conditions the impetus to assure that care is diminished. The class of those who might otherwise protest their lack of care, and choice of alternatives, is diminished and a public demand for better care is diminished as well. The only question has become if a more or less cognitively able person asks for it. But if we wish to promote patient autonomy and freedom of choice the lack of alternatives to medical termination means the choices open to patients are limited. It is, as I argued in 1996, like asking the most vulnerable among us to play “Russian Roulette with a fully loaded revolver”
Koch then argues that MAiD is diminishing equality. He writes:
Finally, promoting MAiD without prior attention to the palliative, rehabilitative, psychological and social services implies that those so in need are somehow unworthy of supportive care that would make an assisted life worthwhile. Medical termination provides both an alternative to the limited care they receive but as well a quick and cost-efficient way to address what might otherwise be a complex and expensive care program. Thus from the perspective of disability the person him or herself is diminished in importance relative to others in the population at large.Based on the lack of real options available to Canadians, Koch challenges the concept of choice. He writes:
The history of MAiD also raises the question of what is meant by autonomy and freedom of choice. That has been the clarion call of advocates from the start but, in the absence of adequate and sufficient clinical and social services what choice is there, really? Typically what is offered is not a balanced and reasonable choice between living and dying “with dignity” (Koch, 2000a) but simply medical termination. These are important issues that are hidden beneath clarion calls for patient choice, autonomy, and freedoms of choice in medical affairs.Koch is stating that since Canada's healthcare system lacks the supports that are necessary to ensure "freedom of choice" as defined by those who support euthanasia. He continues by quoting from former euthanasia leaders in the Netherlands. He writes:
In 1994, Dr. Cornelisse-Claussen, then director of the Dutch Voluntary Euthanasia Society made this emphatically clear: “Everyone here is able to get good health care, and I think only in this context can a law like we have be passed. If the socio-economic circumstances in a country are different, and if there are lots of financial problems with getting good care, then people should be very, very, very careful about introducing these possibilities”. A similar caution was offered, cited in the same article, by Dutch physician Dr. Gerrit Kimsma, an enthusiastic proponent of physician assisted or directed death. "The Netherlands has an extensive primary care system, with universal access with a nursing support that covers 24-hour care for terminal patients.”Koch explains that the US Supreme Court Gluckberg decision shared the same warnings concerning the lack of effective end-of-life care.
Koch concludes that euthanasia proponents Jocelyn Downie and Udo Schuklenk are promoting Canada's euthanasia law as the model for other jurisdictions. This explains why several jurisdictions have debated legalizing Canadian style euthanasia laws. Koch states that if Canada's experience is to be a model for other countries, as Downie and Schuklenk hope, it serves better as a caution than recommendation.
A link to previous articles by ethicist Tom Koch (Link).



No comments:
Post a Comment