Alex Schadenberg
Executive Director, Euthanasia Prevention Coalition
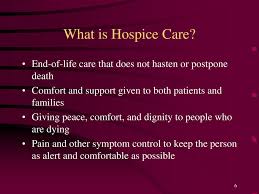
Authentic palliative and hospice care does not hasten death.
O'Neill quotes key people including: Palliative-care expert Dr. Neil Hilliard from Abbotsford BC, Dr. Ebru Kaya, president of the Canadian Society of Palliative Care Physicians, Dr. Leonie Herx, the immediate past president of the Canadian Society of Palliative Care Physicians and myself.
Hilliard, who is a past medical director of palliative care in the Fraser Health BC region stepped back from his role after the BC government demanded that all palliative care facilities (non religiously affiliated) must provide euthanasia. O'Neill quotes Hilliard:
health facilities’ introduction of assisted suicide into palliative-care wards and hospices, following legalization of Medical Assistance in Dying (MAiD) in June 2016, has led to a reduction in true palliative-care services.
“It’s like a cancer growing within the palliative care programs,” said Dr. Hilliard who, in 2017, resigned as medical director of the Fraser Health Authority’s palliative-care program because of his opposition to the authority’s insistence that he support the performing of assisted suicide in hospices.
 |
| Dr Leonie Herx |
“When patients’ palliative care needs are not met, the ensuing physical, emotional and spiritual suffering can lead to them feeling depressed, hopeless, and a burden to others— many of the factors driving requests for MAiD,” Herx said. “Earlier palliative care can alleviate suffering before it becomes irremediable.”
“With almost six years of lived experience now, we have seen significant deleterious effects of the impact of MAiD implementation on palliative care, including diminished resources and increasing distress experienced by palliative care clinicians,” Herx said.
She said some health authorities’ incorporation of euthanasia into palliative care has led to palliative nurses leaving their jobs because they felt unable to provide palliative care. And in Ontario, for example, some hospice palliative care nurse practitioners are using their full-time paid palliative care roles to provide assisted suicide.O'Neill also quotes Dr Kaya from her testimony to the Special Joint Committee on Medical Assistance in Dying who stated:
Moreover, there is “increasing moral distress in palliative care clinicians from forced participation in MAiD due to some health authorities mandating that MAiD be provided in hospices and palliative care units or lose funding,” she said. “This is resulting in retention difficulties and early retirements from palliative care which is accentuating and accelerating the already critical shortage of specialist and generalist palliative care physicians.”
assisted suicide needs to be “distinct and separate” from palliative care to ensure that the latter does not suffer.
“By separating them, palliative care can continue to be the safeguard, as intended,” Kaya said. “MAiD assessors and providers are in a conflict of interest if providing palliative care at the same time. This does not prevent palliative care physicians from practicing MAiD – however they should not be providing palliative alongside MAiD for the same patient.”
 |
| Alex Schadenberg |
governments should stop giving lip service to improving palliative care and should devote more resources to improving it, especially now that MAiD is available.Forcing palliative care facilities to provide euthanasia and assisted suicide (MAiD) has resulted in palliative care medical experts leaving the field, at a time when more end-of-life care is necessary. At the same time it has changed palliative care.
“In my opinion, palliative care has been completely undermined” by MAiD, he said. “I haven’t seen anything to improve palliative care. Even if we had just left palliative care alone, where it could be a safe space, that would have made a big difference.”
People need safe places to die. When BC Ministry of Health defunded the Delta Hospice Society (DHS) for refusing to kill their patients by euthanasia (MAiD) the DHS response was to commit to establish safe places to die in Canada. Groups and individuals who are committed to creating safe places to die need to join with the DHS and work towards this common goal.